Navigating choices for management of Infantile Hemangioma
My daughter has a large compound infantile hemangioma on her neck at the base of her skull. Two and a half years ago I didn’t know what that was, and it's possible you might not either. As it happens, Infantile Hemangiomas are the most common type of vascular lesions, more commonly known as birthmarks, in children. You've probably seen them before and didn't know what they were called, though you might have heard them referred to as strawberry marks, just like I had. Despite how common they are, I feel like calling them a birthmark is actually an anomaly because this kind of lesion is not present at birth, but appears within the first two weeks of life.
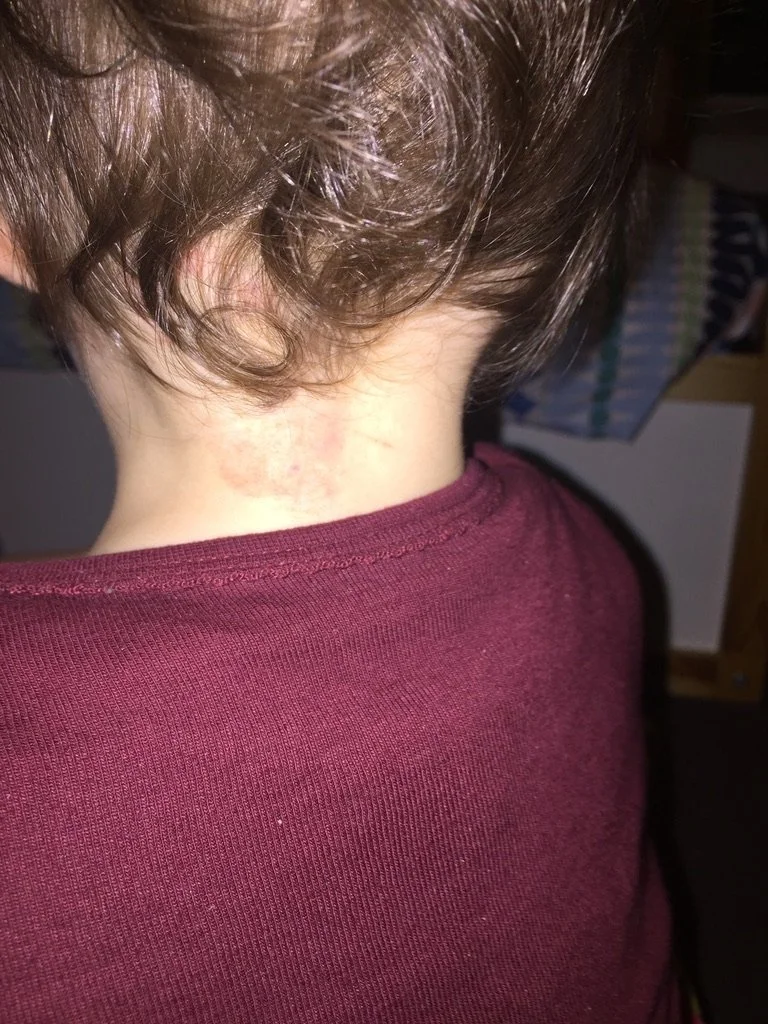
In Lana's case, hers seemed to appear overnight out of nowhere at around 10 days old. There it was suddenly, a small pink patch of skin at the back of her neck. Over the following 6 weeks it grew rapidly from a flat patch about the size of about a ten-cent piece to a large lump equivalent to the size of a large plum. The colour went from pink to deep crimson red and the surface texture gradually changed from smooth to thick and leathery to rough and bumpy. Whilst the lesion was changing before our eyes we spoke to midwives, GPs, and paediatricians all of whom recommended we take the wait and see approach. Generally, this kind of lesion isn't treated as they usually have a natural growth phase of approximately 9-12 months before they enter a dormant phase for several years prior to involuting and eventually reabsorbing back into the body completely by about 7 years of age.
However, each instance of Infantile Hemangioma is different and no-one knows, or was able to reassure us to what extent it would grow before it became dormant. These lesions in themselves are generally harmless although there is a risk of ulceration when they grow very quickly, and just the thought of that happening was horrendous. In cases where Infantile Hemangiomas grow in vital areas such as over an eye, a nasal passage or an airway they are treated to avoid causing secondary problems. So, we waited and waited and while doing so we started noticing that Lana was favouring one side of her neck, always turning the same way. Considering how small she was and how large the lump was on her neck it didn't take long for us to be concerned about it impacting her movement at one of the most crucial periods of her development. We knew that motor development impacts neurological development so we took her to our family chiropractor who tried to encourage her to turn her head the other way but she wasn't very interested in trying, it seemed to take just a little too much effort. We started to become uncomfortable with the wait and see approach so our GP referred us to the dermatology clinic at the Children's Hospital which started a journey that is still ongoing today, two years later.
There was no treatment at all for deep compound Infantile Hemangiomas until 10 years or so ago when a pharmaceutical was discovered purely by chance to deter the growth of these lesions. The drug is a beta blocker usually used for patients with heart problems and while treating young patients with heart disease in France doctors noticed that in children who also had Infantile Hemangiomas, the growth slowed down significantly or stopped while using the beta blockers. Another topical treatment exists these days for superficial lesions but this wasn't going to cut it for Lana so the doctors started talking about putting her on the beta blockers for twelve months to inhibit any further growth. Not surprisingly, we were shocked to suddenly find ourselves having to decide whether to proceed with this treatment or not, for our tiny three-month-old baby. We asked as many questions as we could, sought second opinions and enquired within our hearts and eventually decided that due to the rapid growth and impossibility of knowing how much further it would grow over that first year, we would start treating it.
So, for the next 10 months we gave her two daily doses of the beta blocker and curiously watched as the infantile hemangioma faded and then started to shrink. By about 5 or 6 months into the treatment the lesion had almost become flat against her neck and was a much lighter colour. We were advised to keep her on the treatment until she was twelve months old and when we had a review just after her first birthday, we were told the doctors were super happy with the way the lesion had stopped growing and involuted and it was recommended we stop treatment. So we did, all the while knowing that there was a risk of rebound growth after ceasing treatment but that this was rare after the natural growth period has passed. However, to our dismay it wasn't long before the lesion started to grow back and we were advised once again to wait and see. This was, as at the beginning, the preferred approach as treatment is only recommended in a small number of cases. Over the next 3 months it grew back almost to its largest size again so we were advised to recommence treatment for a further nine months until her second birthday. So we did. Once again, the infantile hemangioma involuted and became almost flat to her neck and when she turned two we were advised once again to cease treatment.
Given our prior experience and how disappointed we anticipated feeling if it were to grow back again and need further treatment, we were initially hesitant to cease treatment the second time around and instead of ceasing abruptly we decided to wean her off the medication slowly. However, despite this approach we started to notice soon after reducing her dosage that the lump was starting to grow back again. So here we are again. Lana is now 2 years and nearly 4 months old and over the past few months we have been seeing the dermatologists monthly to review the regrowth. Once again, we are taking the wait and see approach. They have advised us to do this as they think the regrowth is going to stop by itself which it seems to have done over the past month or so but we are seeking another opinion with a different doctor next month. I have been wanting to write about our experience as parents of a child with a large compound Infantile Hemangioma for quite a while but it just hasn't felt like the right time. It does now.
Lana has become aware of her lesion (which she can't see as it's right behind her neck) mainly through us regularly photographing and analysing it. I also have a tendency to cup my hand over it to cradle it almost and she has started to do the same. We call it her special strawberry and although she doesn't seem particularly interested in it, she enjoys any attention she gets, like most children do. We were lucky that her lesion never ulcerated (as they sometimes do, which is awful for all involved) during its initial rapid growth phase and hasn't, to our knowledge, really caused her discomfort since, other than a couple of times when she fell back on it directly and bumped it which resulted in some nasty bruising given the extensive additional vascular network that makes up its composition. Although in some instances the side effects to the medication she has been on are moderate to serious, she only appeared to display mild side effects such as cold extremities, due to the medication slowing the circulation.
In the early days of navigating this experience I found great comfort in the support of other parents on similar journeys through a Facebook group for parents of children with Infantile Hemangiomas. This global network of parents answered my questions and reassured me when trying to decide what to do and I found great solace in the experiences they shared. I have found it interesting over the past couple of years to observe the different ways people react to Lana's lesion. Some asked if she had been bumped, some stared and didn’t say anything, and some asked what it was. I personally always liked when they asked as it gave me an opportunity to tell them and explain that Lana was being treated for it but that she wasn't even aware of it. I've kept photos on the camera roll of my phone to show people what it looked like when it first appeared as well as at its largest size before we started treatment the first time and I've found that most people tell me they didn't know birthmarks can look like that and grow like that at all. Just like I hadn’t known, so there has at least been some awareness spread through out experience.
I hope this might help other parents starting to navigate the decision-making process around management of Infantile Hemangioma, through those early days of trying to devour all of the information and case studies they can find. It might also be useful to early childhood workers or doctors or birth workers who are also often lacking knowledge of this kind of lesion. I know in the United States, there tends to be a more hands on active approach and these lesions are often removed via surgery. When we enquired about that here (when Lana was still a baby) we were told that due to the location on her neck, surgery came with a risk of bleeding to death (yes, they actually said that).
Update several years later, Lana is now nearly 6.5 years old, although the lesion seems to be gradually reducing in size, it is still very prominent, especially when her hair is wet. Other children ask her about it but she replies very matter of factly, simply telling them it is her birthmark. However, we’ve always been keen to see if she becomes self conscious about it as she gets bigger. Every time we’ve discussed the possibility of having it removed (which we’ve been since told is actually a safe choice if she chooses to make it), she gets protective of it and says she doesn’t want to, so we’re taking her lead, we’ll see where this journey leads for her.
If you know anyone who you think may be interested, please share this blog with them; if you have any questions, please ask me; if you have a similar experience that you'd like to share with me, please do so. The more we talk about Infantile Hemangiomas the more people will know what they are, and what they're not.
If you enjoyed reading this Blog and would like to learn more of my story, come over to find me on IG @marygiordano.com.au